The use of patient data is a growing, complex and often contested topic. This page - for journalists and others writing about the topic - provides a brief overview of the history of patient data along with information about the role of the media in reflecting and shaping public debate around health data.
In addition to this page, our media hub contains a summary of public attitudes, tips for writing about health data, and links to further resources.
Whilst this web page is relevant across the four nations of the United Kingdom, many of the examples discussed focus on England given the prominence of the debate around patient data in England. Where possible, we have indicated what country we are talking about.
The big picture: what drives the debate?
A complex policy and programme landscape
Health data policy is complex and developing at speed to support a multitude of new and emerging programmes alongside rising public expectations of transparency and choice. Ongoing discussions include:
- How opt outs should work (whether National Data Opt Out, Type 1 Opt Out or others)
- Who owns the data
- Who can access the data
- What a fair commercial partnership looks like
Diffused leadership with unclear lines of accountability
Diffused national leadership, accountability and governance (i.e. across Government, shifting NHS and arms-length bodies) has resulted in siloed and uncoordinated engagement with national stakeholders and with front line staff, including GPs.
Misinformation, distrust and speculation thrive in the absence of consolidated national leadership of this agenda.
Low public awareness and understanding
Historically non-existent or cursory national engagement with the public and patchy regional engagement means awareness of how data is used is so low that informed choice isn't really possible and trust is tenuous at best. This often leads to people opting out of sharing their health data - a natural response to media stories highlighting risks without context.
Whilst there has been an increase in national communications about patient data in recent years, awareness and understanding remains low.
Negative media coverage focused on risk
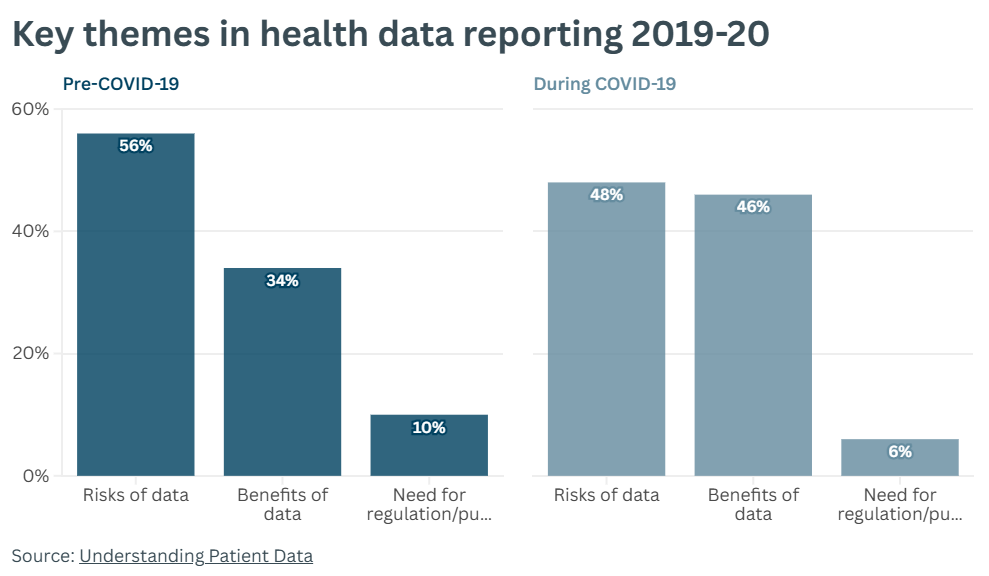
An analysis of media coverage of health data stories in 2019-20 commissioned by Understanding Patient Data showed that:
- Stories about the risks of using health data received the most attention. The media usually only analyses the way health data is collected, stored and used when something goes wrong (like a data breach). These stories have the most cut-through with the public, leading to a big focus on risks in public conversation.
- Stories about health data are highly politicised and often tied to broader issues, like elections, privatisation of the NHS or the ways tech companies use data.
- Positive stories about new treatments or breakthroughs in health research rarely explain the role of health data, meaning positive coverage does not increase public awareness of the importance of health data
- Individuals are generally positioned as passive players and there is limited focus on the role individuals can play in managing data about their health. This is likely to be increasing sentiments like anger and fear in public conversation if people feel they don’t have any control over data about them.
The graph below shows that a majority of media coverage prior to COVID-19 focused on the risks of health data, though this became more balanced during the pandemic.
History: patient data initiatives to date
The current conversation about patient data does not exist in a vacuum, and is affected both by the history of developments past, and how these developments have been covered in the media.
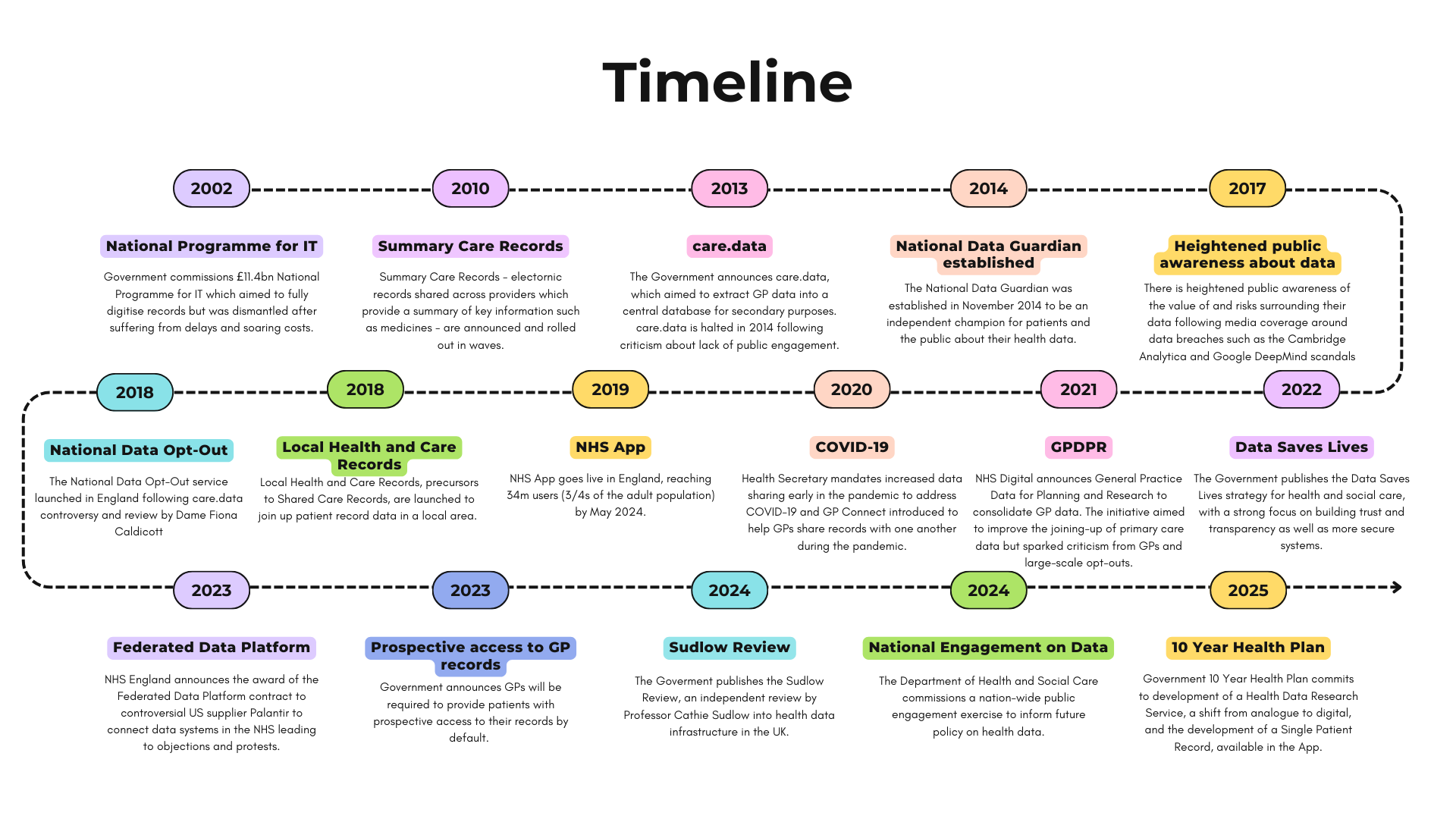
Media: how media coverage drives the debate
Particularly in England, reporting on health data initiatives has often focused on the risks of using data. This, coupled with lobbying from privacy campaigners and parts of the medical profession, has led to media coverage about patient data leaning negative and further increasing public skepticism.
Over the past decade, UK media coverage has helped highlight legitimate public concerns and exposed real issues in relation to the use of health data — but has also:
- Been a contributing factor to the collapse of national programmes (care.data, GP Data for Planning and Research)
- Heightened concerns around private sector and international access to data
- Amplified public anxiety over cyber breaches and misuse
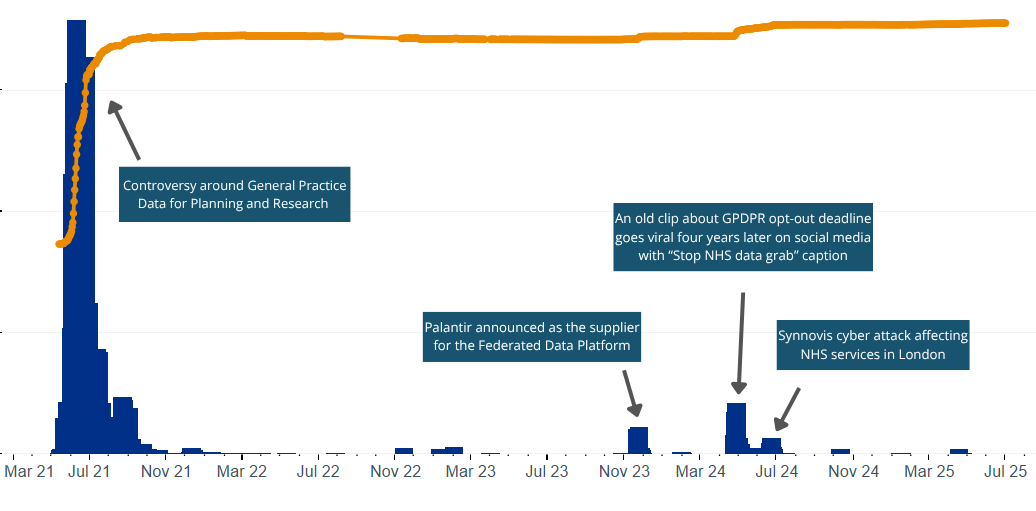
A graph showing the National Data Opt Out (below) with areas of controversy in the media overlaid demonstrates the close relationship between media coverage and opt-out behaviour (which can be seen as a proxy for public distrust in the management of patient data).
Why this matters:
- Media coverage shapes public trust and government decisions (from policy to practice)
- Sensational stories about privacy, profit, and misuse dominate over more positive ones
- Inaccurate or unbalanced reporting can fuel mistrust, put data initiatives to a halt and lead to people opting out of data-sharing. This slows efforts to realise the life-saving potential of health data
Examples of coverage about health data in the media
The impact
Controversy around patient data initiatives and the nature of media coverage on the topic have several impacts on the conversation around health data:
Higher Opt-Out rates
Higher Opt-Out rates reflect diminished trust, and as shown in the section above, there is an association between moments of heightened media interest in patient data and higher Opt-Out rates. More people opting out shrinks the amount of data available for research and service planning, reducing confidence in the results. Read more about opting out and Opt-Out rates in England.
Distorted data
Opt-outs are not evenly distributed and vary by geography and demographics. For instance, women are more likely to opt out than men (6.2% vs 4.9%) and the Opt-Out rate is higher in London (7.1%) than in the North East and North Yorkshire (4.3%). This makes data less representative, distorting findings and risking the exclusion of certain groups from research and services. This is particularly an issue as researchers conducting health research do not know who has opted out and therefore do not know how well the dataset they have reflects the whole population they wish to study.
Wasted investment
Public backlash can lead to paused or abandoned programmes, wasting significant public funds. For instance, the National Programme for IT cost £10bn, whilst care.data cost £8m, both of which were eventually abandoned. Whilst the demise of these programmes was not solely driven by public opinion, declining public trust and media backlash both play a part.
Risk aversion
Policymakers and data users may become reluctant to engage on complex or controversial issues or invest capital (both political and financial) into reforms or policy programmes related to patient data out of fear of backlash in the media or among the public. This reluctance to engage may lead to missed opportunities to improve care.
Learn more
For more information for journalists and others writing about health data, please consult our media hub with further resources.
